An oophorectomy, also known as ovary removal surgery, is a surgery many people undergo for different health reasons—sometimes as part of treatment, other times as a preventive measure. If you’re preparing for this procedure or simply exploring what it might mean for you, it’s normal to have questions. Below, we’ll walk through what an oophorectomy involves, what happens when your ovaries are removed, and what recovery can look like—so you can move forward with confidence and take an active role in your care.
What is an oophorectomy?
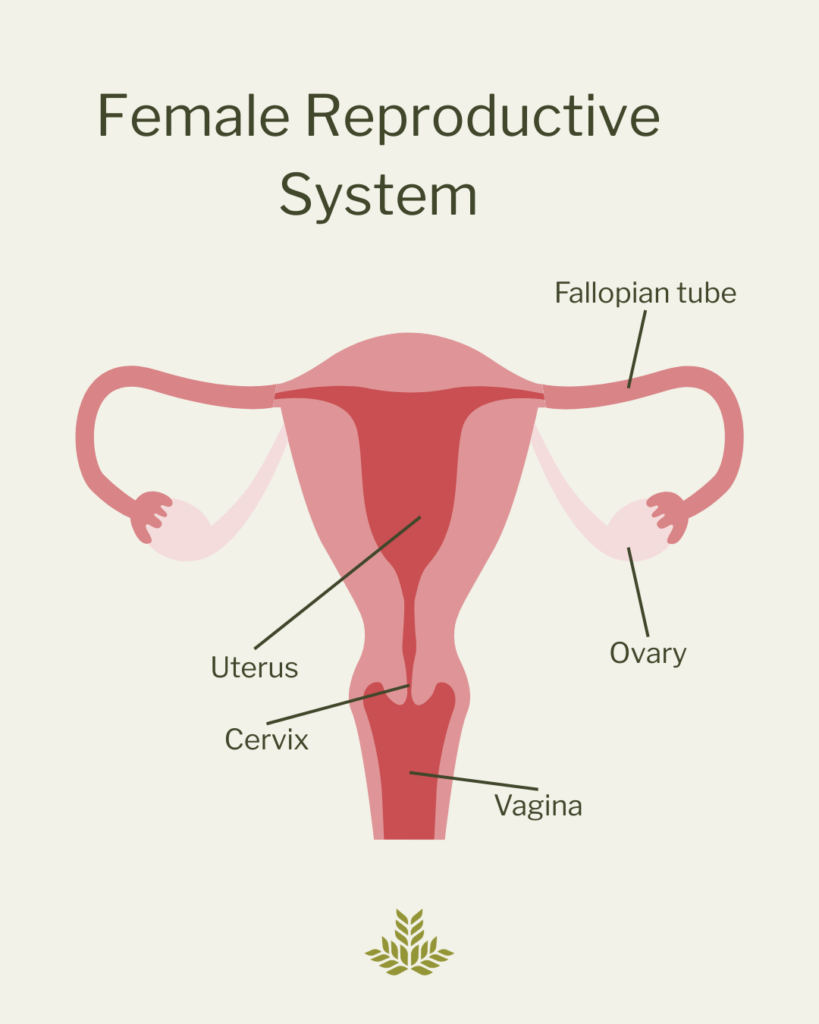
An oophorectomy is a surgery to remove one or both of your ovaries. Ovaries are small, almond-shaped organs located on either side of the uterus. They play an important role in producing reproductive hormones—estrogen and progesterone—and in releasing eggs through the fallopian tubes.
Types of oophorectomies
There are several types:
- Unilateral: one ovary removed
- Bilateral: both ovaries removed
- Salpingo-oophorectomy : one or both ovaries and fallopian tube(s) removed
- Hysterectomy with salpingo-oophorectomy: uterus, fallopian tubes and ovaries removed
Why is ovary removal surgery done?
Your doctor may recommend this surgery for multiple reasons, including:
Ovarian cysts or tumors
Most ovarian cysts are harmless, but if they’re large, painful, or don’t go away on their own, your doctor may recommend removing the affected ovary—especially if there’s concern the cyst could be cancerous or cause other problems.
Ovarian cancer or high risk of cancer
If you’ve been diagnosed with ovarian cancer, or if you carry a genetic mutation like BRCA1 or BRCA2 that puts you at high risk, your doctor may recommend removing one or both ovaries to treat or prevent the disease.
Endometriosis
This condition causes tissue similar to the lining of the uterus to grow outside of it, sometimes affecting the ovaries. In severe cases that haven’t improved with other treatments, removing one or both ovaries may help reduce pain and symptoms.
Ovarian torsion
This happens when an ovary twists on itself, cutting off its blood supply. It’s a medical emergency, and sometimes the ovary can’t be saved. Surgery may be needed to remove it and prevent further complications.
Tubo-ovarian abscess
A tubo-ovarian abscess is a pocket of infection involving the ovary and fallopian tube. If it doesn’t respond to antibiotics or becomes too large, surgery may be needed to remove the infected tissue and prevent the infection from spreading.
In some cases, an oophorectomy is done along with another procedure, like a hysterectomy(removal of the uterus), especially if you’re already having surgery for a related issue.
What happens when my ovaries are removed?
The ovaries are responsible for producing estrogen and progesterone – reproductive hormones that play a vital role in multiple systems of the body. Estrogen helps regulate your menstrual cycle, supports vaginal and urinary health, protects bone strength, and contributes to heart and brain function. Progesterone helps prepare the uterus for pregnancy and supports early pregnancy, but it also has calming effects on the brain and helps balance estrogen.
When one or both ovaries are removed, your levels of these hormones drop—sometimes dramatically—especially if both ovaries are taken out. That sudden loss of hormones leads to a variety of physical and emotional changes.
Hormonal Changes
Without estrogen and progesterone, you may experience symptoms such as:
- Hot flashes
- Night sweats
- Mood swings or irritability
- Vaginal dryness
- Trouble sleeping
These are often referred to as menopausal symptoms, and they may come on quickly after surgery if both ovaries are removed.
Menopause
If you haven’t gone through menopause yet, removing both ovaries will cause it to happen suddenly. This is known as surgical menopause, and its symptoms are often more intense than natural menopause because the hormonal shift is immediate.
Fertility Impact
Ovary removal also affects fertility. If both ovaries are removed, you will no longer produce eggs and won’t be able to get pregnant naturally. However, if only one ovary is removed and is healthy, the remaining ovary may continue to function—and pregnancy is still possible.
Long-Term Considerations
Because estrogen does more than regulate reproduction, its loss from ovary removal has long-term health effects:
- Bone health: Estrogen helps maintain bone density, so lower levels increase the risk of osteoporosis.
- Heart health: Estrogen also supports healthy cholesterol levels and blood vessels, so its absence may increase heart disease risk.
If you are experiencing surgical menopause after having both of your ovaries removed, hormone replacement therapy may be an option to alleviate your symptoms and protect your bone and heart health. Speak with your physician to see if this is the right treatment for you.
What to expect during surgery
There are a few different approaches your surgeon might use for your oophorectomy. The approach depends on your health history, the reason for surgery, and whether additional procedures—like a hysterectomy—are being done at the same time.
- Laparoscopic – This minimally invasive option uses a few small incisions and a tiny camera (laparoscope) to guide the procedure. Most people experience less pain and faster recovery with laparoscopic oophorectomy.
- Open Abdominal – In some cases, a larger incision is needed in the lower abdomen—especially if there’s concern about cancer, large masses, or scar tissue from previous surgeries. Recovery time is typically longer with this approach.
- Robotic Assisted Laparoscopic – Like a traditional laparoscopy, but with enhanced precision using robotic instruments controlled by your surgeon. This method can offer greater accuracy for complex cases.
What will recovery look like after an oophorectomy?
Recovery after an oophorectomy is a gradual process, and it can look a little different for everyone. While there’s no exact timeline, most people move through a few general stages as they heal:
- Rest and healing: At first, you’ll likely feel tired and sore as your body begins to recover. Common symptoms during this early phase include abdominal or pelvic discomfort, bloating or gas, light vaginal bleeding, and general fatigue. Gentle movement, like short walks, can help with circulation and ease some symptoms.
- Returning to light activity: As you start to feel better, you may be able to resume light daily tasks. You might still feel tender or low on energy, and that’s completely normal. Be sure to avoid heavy lifting or anything that causes strain until your doctor gives you the all-clear.
- Resuming normal routines: Over time—and with guidance from your care team—you can gradually return to your regular routines. This might include work, exercise, or other physical activity. Everyone’s pace is different, so it’s important to listen to your body and not rush the process.
Some days may feel better than others. If anything doesn’t feel right, or if your symptoms seem to worsen instead of improving, don’t hesitate to reach out to your doctor.
When to Call Your Doctor
Reach out right away if you experience:
- Fever or signs of infection
- Severe pain or swelling
- Heavy vaginal bleeding
- Trouble urinating or moving your bowels
- Intense mood swings or emotional distress
FAQs About Oophorectomy
Is oophorectomy a major surgery?
Yes, though often minimally invasive, it’s still considered major surgery.
Can I get pregnant after a unilateral oophorectomy?
Yes, if one ovary remains and is healthy.
Will I go into menopause right away?
Only if both ovaries are removed and you haven’t gone through menopause already.
What are the risks?
Like any surgery: bleeding, infection, or reaction to anesthesia. Long-term, there’s also risk tied to sudden hormonal changes.
Is hormone therapy required?
Not always—but it’s often recommended to manage symptoms and protect heart and bone health.
Final thoughts
An oophorectomy is a big step, but you don’t have to face it alone. Recovery takes time, and it’s okay to have questions or concerns along the way. At Northeast Georgia Health System, we’re here to support you before, during and after surgery—with expert care and resources to help you heal, adjust and move forward with confidence.



